What is the cornea?
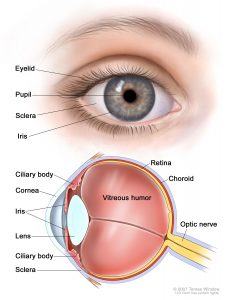 The cornea is the transparent, dome-shaped, outermost layer that covers the iris and pupil in the front of the eye. Corneal tissue consists of five basic layers: epithelium, Bowman’s layer, stroma, Descemet’s membrane and endothelium. Although the cornea is clear, it contains a highly organized group of cells and proteins. Unlike most tissues in the body, the cornea contains no blood vessels to nourish or protect it against infection. Instead, the cornea receives its nourishment from the tears and aqueous humor that fill the chamber behind it.
The cornea is the transparent, dome-shaped, outermost layer that covers the iris and pupil in the front of the eye. Corneal tissue consists of five basic layers: epithelium, Bowman’s layer, stroma, Descemet’s membrane and endothelium. Although the cornea is clear, it contains a highly organized group of cells and proteins. Unlike most tissues in the body, the cornea contains no blood vessels to nourish or protect it against infection. Instead, the cornea receives its nourishment from the tears and aqueous humor that fill the chamber behind it.
The cornea, one of the protective layers of the eye, serves two functions:
First, along with the eyelid, eye socket, and sclera (white part of the eye), and the tear film, the cornea shields the eye from dust, germs, and other harmful matter.
Second, as the eye’s outermost lens, it is the entry point for light into the eye. When light strikes the cornea, it bends, or refracts, the incoming light onto the lens. The lens further refocuses the light onto the retina, a layer of light-sensing cells lining the back of the eye.
To see clearly, the cornea and lens must focus the light rays precisely on the retina. This refractive process is similar to the way a camera takes a picture. The cornea and lens in the eye act as would a camera’s lens. The retina approximates the film. If the cornea is unable to focus the light properly, then the retina receives a blurry image.
What is keratoconus and corneal ectasia? 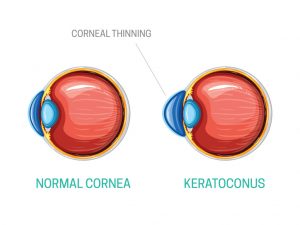
Keratoconus means “conical or cone-shaped cornea”. It is a disease in which the cornea stretches or bulges forward into a cone-like shape. Because the cornea is the major focusing surface of the eye the shape change causes blurred and distorted vision. The normal physical properties of the cornea are altered, and this causes a refractive error; usually short-sightedness (myopia) and irregular astigmatism.
Diagnosis of keratoconus is based on thinning of the cornea at the apex of the cone (found on slit-lamp examination) and corneal topographic and keratometric assessment of the curvature of the cornea. Keratoconus commonly affects children and young adults. This stretching or bulging of the cornea tends to progress but the rate at which it does vary. It usually affects both eyes but can be asymmetrical.
The first line of treatment is usually with rigid contact lenses, although some people with early keratoconus may be able to wear spectacles or soft contact lenses. Good vision in patients with keratoconus may be difficult to maintain. As the disease progresses, spectacles or contact lenses may not be sufficient to correct vision. Lamellar keratoplasty or penetrating keratoplasty may be required for severe progressive forms of the disease.
Recently, corneal collagen cross-linking has emerged as the gold standard treatment to halt progression of keratoconus.
What is collagen cross-linking?
First developed in Germany in 1998 and progressively improved on since then corneal collagen crosslinking (C3R or UV-X) uses ultraviolet light and riboflavin eye drops (vitamin B2) to stiffen the cornea. It works by cross-linking the protein fibres in the cornea to each other and within themselves. This procedure has been used in the early stages of keratoconus as a way of halting the progression of the disease. Collagen cross-linking mimics the corneal stiffening which occurs naturally with ageing. This is the reason why keratoconus does not usually progress in people aged 50 and over.
What does the procedure involve?
The procedure is performed as an outpatient procedure using topical anaesthetic eye drops. A speculum is placed to keep the eye open during the procedure. The epithelium is first removed to allow the penetration of riboflavin into the corneal tissue. Riboflavin eye drops are applied frequently to the corneal surface while the cornea is exposed to 30 minutes of ultraviolet-A radiation. A soft bandage contact lens is placed on the eye at the end of the procedure.
